(Reuters) - U.S. President Joe Biden's administration on Wednesday finalized a rule requiring health insurers to set time targets for the prior authorization process for patients seeking approval for medical services under government-backed insurance plans.
The Centers for Medicare & Medicaid Services (CMS), a division of the Department Of Health And Human Services, said the rule will begin primarily in 2026.
The rule applies to health insurance companies providing government backed-insurance plans such as Medicare for those aged 65 and above, and the Medicaid plan for low-income individuals.
Some physician organizations in recent years have pushed back against the use of prior authorizations, which they say increased the paperwork for doctors and leads to restrictive coverage in some cases.
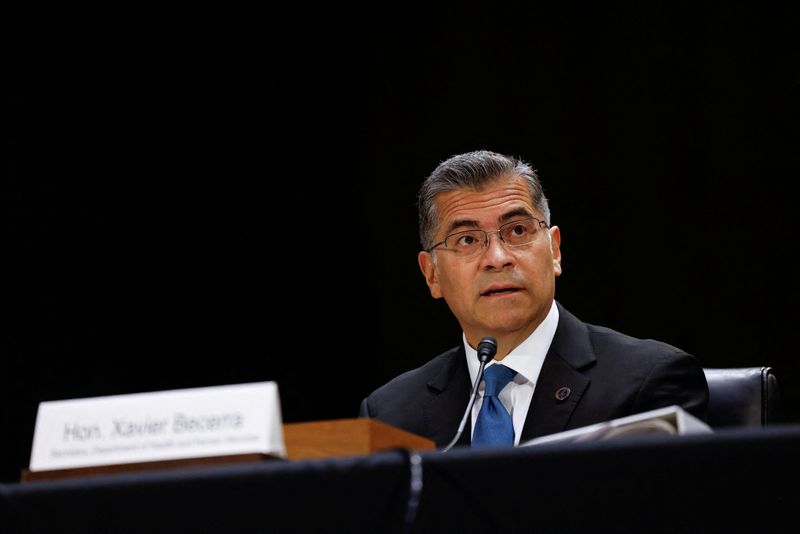
"When a doctor says a patient needs a procedure, it is essential that it happens in a timely manner," Health and Human Services Secretary Xavier Becerra said. "Too many Americans are left in limbo, waiting for approval from their insurance company."
Under the new rule, prior authorization decisions are required to be sent within 72 hours for urgent requests, and seven calendar days for standard non-urgent requests.
For some insurers, the new timeframe for standard requests cuts current decision time in half, according to the CMS.
It also requires all payers to include a specific reason for denying a prior authorization request, which will help re-submissions of the request or an appeal when needed.
UnitedHealth Group (NYSE:UNH)'s insurance unit as well as health insurer Cigna (NYSE:CI) said last year they would cut down the use of prior authorization.