- UnitedHealth absorbs $720 million loss courtesy of Obamacare
- Management is mulling pulling out of Obamacare as losses mount.
- Portion of the $9.5-$10 billion cash flow in 2016 could trickle down to shareholders through buybacks.
UnitedHealth Group Inc (NYSE:N:UNH) is expecting more losses in its Affordable Care Act (ACA) plans in 2016. The U.S. leading insurer registered a loss of $720 million through ACA in 2015. The management of UnitedHealth is currently weighing options of whether to withdrawal or stay in ACA business. Exiting ACA, or fondly the Obamacare, appears to be a popular option, although the company might still maintain some presence in ACA plan, but at a greatly reduced exposure.
After booking a loss of $720 million courtesy of Obamacare in 2015, UnitedHealth Group Inc (NYSE:UNH) is projecting that its Obamacare-linked losses in 2016 could exceed $500 million, which is above the initial management estimate for a loss between $400 and $425 million. The reason UnitedHealth is modeling a steeper Obamacare loss in 2016 than it previously guided is that its Obamacare enrollment for this year surpassed expectations. The company tried to suppress its Obamacare enrollment by trimming marketing and commissions to agents, but all that failed to put off people signing up for the ACA coverage through the insurer.
Because of the ACA issue, it may seem that there is nothing more to be excited about UnitedHealth, but nothing can be further from the truth. Although health insurance is UnitedHealth’s largest business, the management is expressing confidence that Optum unit will drive growth despite the rot in the ACA coverage and offset challenges elsewhere.
ACA pain should be short-lived
It looks likely that UnitedHealth’s assessment of its Obamacare coverage will favor exit from the plan. However, the company might retain a small presence in the plan if it must, which should reduce its exposure to Obamacare losses.
UnitedHealth added 70,000 enrolling to its register for 2016, a number more than 55,000 it signed up in 2015. The management tried to discourage Obamacare individual signup in 2016 through means such as reducing ACA-themed marketing, dropping some production options and cutting commissions for agents. Unfortunately, signups still surged beyond expectation, leading management to conclude that 2016 ACA losses will be $100 million more than the loss previously guided for the year. As such, UnitedHealth is preparing to absorb more than $500 million in Obamacare-related losses in 2016.
However, because the company is mulling exit from the loss ACA coverage, its woes related to the plan should ease over time and eventually go away. Currently, the management is considering whether there is any reason for UnitedHealth to continue Obamacare coverage in 2017.
Strong guidance despite Obamacare challenge
UnitedHealth Group Inc (NYSE:UNH) is expecting EPS of $7.60-$7.80 on revenue of $180 billion in 2016. You can see that the management expects the company to continue generating profits despite the anticipated huge loss in the Obamacare plan. Perhaps that begs the question about where UnitedHealth is drawing its confidence.
Optum business
Amid challenges in Obamacare plan, UnitedHealth Group Inc (NYSE:UNH) is finding support in its Optum business, a unit that renders a bevy of health services. The unit has been growing at a decent rate and has been offsetting the losses in health insurance business. In 4Q, Optum business revenues rose 70% to hit $21.9 billion, accounting for 50% of UnitedHealth’s total revenues in the quarter. Optum’s prescription arm was the bright spot in 4Q. That growth trend is expected to continue this year and into the future as UnitedHealth continues to invest in growth in the unit.
Stocking Optum
UnitedHealth has not only been relying more on Optum to underwrite health insurance losses, but the company has also been investing in the growth of the unit. The acquisition of Catamaran, a pharmacy-benefit manager, has raised the profile of the Optum business, opening opportunities in new business segments for more accelerated growth.
Today, UnitedHealth boasts that Optum owns and operates over 270 clinic locations in 26 markets in the U.S. With that network, the business serves over 7 million patients through its network of more than 150 payer partners.
There is a feeling at UnitedHealth that Optum has barely scratched the surface of its available opportunity. That means that continued investment in the business should unlock more revenues and profits.
Among other things, UnitedHealth provides technology services, offers PBM services and operates clinics through its Optum business.
Shareholder returns
UnitedHealth Group Inc (NYSE:UNH) repurchased its shares worth between $60 and $65 million in the last quarter, thus reducing its outstanding shares by 600,000 in the quarter. For the year 2015, the company bought back 10.7 million shares, spending $1.2 billion in buybacks for the year. Although UnitedHealth is facing issues in its health insurance business and has slowed shares repurchases, the management remains committed to returning value to shareholders.
With the management of UnitedHealth modeling 2016 cash flow in the range of $9.5-$10 billion, part of that amount should go into deleveraging the balance sheet post the Catamaran buyout. Some of that free cash flow is also expected to find its way back into the pockets of shareholders through shares buybacks.
4Q2015 results highlight
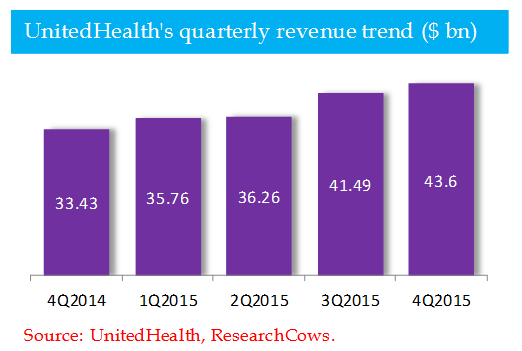
UnitedHealth Group Inc (NYSE:UNH) still managed to post a profit in 4Q2015 despite the $245 million loss associated with Obamacare. Net income of $1.22 billion or $1.26 per share was mainly supported by gains in the Optum unit. Adjusted EPS of $1.40 surpassed the consensus estimate of $1.38 but fell short of $1.64 in the same period a year earlier. Revenue of $43.60 billion rose 30% YoY, topping the consensus estimate of $43.23 billion.
The chart below depicts UnitedHealth’s revenue trend over the last five quarters:
Bottom line
The noise generated by Obamacare losses need not cloud the bigger picture in UnitedHealth Group Inc (NYSE:UNH). As the management thinks of what to do with its Obamacare business, Optum can be relied upon to keep the business growing. Once the Obamacare issue is resolve, UnitedHealth should see more accelerated topline and bottom-line growth.
Disclaimer: The opinions and data expressed herein by the author are not an investment recommendation and are not meant to be relied upon in investment decisions. The author is not acting in an investment advisory capacity, nor is this an investment research report. The author’s opinions expressed herein address only select aspects of potential investment in securities of the company or companies mentioned and cannot be a substitute for comprehensive investment analysis. Any analysis presented herein is illustrative in nature, limited in scope, based on an incomplete set of information, and has limitations to its accuracy. The author recommends that potential and existing investors conduct thorough investment research of their own, including detailed review of the companies’ SEC filings, and consult a qualified investment advisor. The information upon which this material is based was obtained from sources believed to be reliable, but has not been independently verified. Therefore, the author cannot guarantee its accuracy. Any opinions or estimates constitute the author’s best judgment as of the date of publication, and are subject to change without notice.
